I have had several tooth adventures. The time I rather enthusiastically pushed my middle sister on her bicycle and she fell over the handlebars breaking a tooth (or was that the time I helped her break her collar-bone?). My own dental fluorosis (a developmental disturbance of enamel that results from ingesting high amounts of fluoride during tooth mineralization) and my mother’s sobering experience of periodontal disease. Not to mention my parents’ adventures in dental tourism, but I’ll save those for another time.
Apart from the personal injunction to clean and floss my teeth, I didn’t think too much about oral health as a mental health clinician until I’d left clinical practice for education, when I found myself at AUT University in a faculty committed to inter-professional education and practice, where “current or future health professionals to learn with, from, and about one another in order to improve collaboration and the quality of care.”
We had learned about oral health as undergraduate nurses, particularly about post-operative oral health care and oral health for older people. But even when working in acute mental health units, community mental health and maternity, I hate to admit, oral health wasn’t on my mind. Unsurprisingly, evidence shows that even though oral health is a major determinant of general health, self esteem and quality of life, it often has a low priority in the context of mental illness (Matevosyan 2010).
As the programme leader of health promotion at AUT, a colleague in the oral health team asked me to talk to her students about the connections between mental health and oral health and that’s when my journey really began. I also had the pleasure of getting my teeth cleaned and checked at the on site Akoranga Integrated Health at AUT whose services were provided by final year and post graduate health science students under close supervision of a qualified clinical team.
It made me think about how oral health care is performed in a highly sensual area of the body. I learned that oral tissues develop by week 7 and the foetus can be seen sucking their thumb. It made me think about how suckling and maternal bonding are critical after birth. It made me think about how we use our mouths to express ourselves and to smile or show anger or shyness, literally 65% of of our communication. It made me think about kissing in intimate relationships and therefore also about how it’s not at all surprising that our mouths also represent vulnerability and that people might consequently suffer from fear and anxiety around oral health treatment. This can range from slight feelings of unease during routine procedures to feelings of extreme anxiety long before treatment is happening (odontophobia). Reportedly, 5-20% of the adult population reports fear or anxiety of oral health care, which can lead to avoidance of dental treatment and common triggers can include local anaesthetic injection and the dental drill.
Poor oral health has a detrimental effect on one’s quality of life. Loss of teeth impairs eating, leading to reduced nutritional status and diet-related ill health. A quarter of Australians report that they avoid eating some foods as a consequence of the pain and discomfort caused by their poor dental health. Nearly one-third found it uncomfortable to eat in general. Oral disease creates pain, suffering, disfigurement and disability. Almost one-quarter of Australian adults report feeling self-conscious or embarrassed because of oral health problems, impacting on enjoyment of life, impairing social life or leading to isolation with compromised interpersonal relationships
People with severe mental illness are more likely to require oral health care and have 2.7 times the general population’s likelihood of losing all their teeth (Kisely 2016). Women with mental illness have a higher DMFT index (the mean number of decayed, missing, and filled teeth) (Matevosyan 2010). In particular, oral hygiene may be compromised. For people who experience mood disorders, depressive phases can leave person feeling worthless, sad and lacking in energy, where maintaining a healthy diet and oral hygiene become a low priority. The increased energy of manic episodes can mean energy is diffused, concentration difficulties and poor judgement. People who experience mental ill health and who self-medicate with recreational drugs and alcohol can further exacerbate poor oral health. Furthermore, drug side effects can compromise good oral health by increasing plaque and calculus formation (Slack-Smith et al. 2016). It is important for mental health support staff to provide information regarding oral health, in particular education about xerostomic (dry mouth) effects of drug treatment and strategies for managing these effects including maintaining oral hygiene, offering artificial saliva products, mouthwashes and topical fluoride applications.
There are organisational and professional barriers to better oral health in mental health care. Mental health nurses do not routinely assess oral health or hygiene and lack oral health knowledge or have comprehensive protocols to follow. As Slack-Smith et al. (2016) note there are few structural and systemic supports in care environments with multiple competing demands. Research shows that dentists are more likely to extract teeth than carry out complex preventative or restorative care in this population. Mental health clinicians are reluctant to discuss oral health and in turn oral health practitioners are not always prepared for providing care to patients with mental health disorders.
Which brings me to the topic of this blog post. Until the 17th century, medical care and dental care were integrated, however, dentistry emerged as a distinct discipline, separate from doctors, alchemists and barbers who had had teeth removal in their scope of practice (Kisely 2016).
I spent the weekend at the Putting the Mouth Back into the Body conference, an innovative, multidisciplinary health conference hosted by North Richmond Community Health. It got me thinking about the place of the mouth in the body and developed my learning further. The scientific method and the mechanistic model of the body central to the western biomedical conception of the body, have led us to see the body in parts which can be attended to separately from each other. And yet we know what affects one part of the body affects other parts. There’ll be an official outcomes report produced from the conference, but I thought I’d capture some of my own reflections and learning in this blog post.
Equity and the social determinants of dental disease
Tooth decay is Australia’s most prevalent health problem with edentulism (loss of all natural teeth) the third-most prevalent health problem. Gum disease is the fifth-most prevalent health problem. Tooth decay is five times more prevalent than asthma in children. Oral conditions including tooth decay, gum disease, oral cancer and oral trauma create a ‘burden’ due to their direct effect on people’s quality of life and the indirect impact on the economy. There are also significant financial and public health implications of poor oral health and hygiene. Hon. Mary-Anne Thomas MP, Parliamentary Secretary for Health and Parliamentary Secretary for Carers spoke about the impact of oral health on employment. She reinforced research findings which show that people with straight teeth as 45 per cent more likely to get a job than those with crooked teeth, when competing with someone with a similar skill set and experience. People with straight teeth were seen as 58 per cent more likely to be successful and 58 per cent more likely to be wealthy. Dental health is excluded from the Australian Government’s health scheme Medicare, which means that there is significant suffering by those who cannot afford the cost of private dental care for example low-income and marginalised groups. Dental care only constitutes 6% of national health spending and comprehensive reform could be effected with the addition of less than 2 percentage points to this says a Brotherhood of St Lawrence report (End the decay: the cost of poor dental health and what should be done about it by Bronwyn Richardson and Jeff Richardson (2011)). The socially
disadvantaged also experience more inequalities in Early Childhood Caries (ECC) rates. Research has also shown that children from refugee families have poorer oral health than the wider population. A study by my colleagues at North Richmond Community Health and University of Melbourne found that low dental service use by migrant preschool children. The study recommended that health services consider organizational cultural competence, outreach and increased engagement with the migrant community (Christian, Young et al., 2015).
The interactions between oral health and general health
Professor Joerg Eberhard spoke about the interactions between oral and general health through the lifespan. His talk also demonstrated the importance of oral hygiene, not only to prevent cavities and gum disease but impact on pregnancy, diabetes and cardiovascular health. 50 to 70 per cent of the population have gingivitis and severe gum disease (periodontitis) which develop in response to bacterial accumulation have adverse effects for general health. He showed participants the interactions of oral health and general health with a focus on diabetes mellitus, cardiovascular disease and neurodegenerative diseases. Most strikingly, Eberhard’s research published in The International Journal of Cardiology in 2014, showed periodontitis could undermine the major benefits of physical activity. If you are interested in the link between oral health and non-communicable diseases, this Sydney Morning Herald article provides a great summary.
Key points:
- What effects the body also affects the mouth, in fact this is bidirectional.
- Early experiences impact lifelong health eg sugar preference, early cavities, diet.
Sugar is a significant culprit
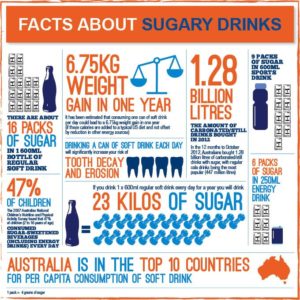
I learned a lot about sugar from Jane Martin the Exective Manager of the Obesity Policy Coalition and Clinical Associate Professor Matthew Hopcraft an Australian dentist, public health academic and television cook. 52% of Australians exceed the WHO recommendations for sugar intake, and half of our free sugars come from beverages. Sugar intake profoundly impacts cavities and our contemporary modes of industrial food production are to blame. We also need to challenge the subtle marketing of energy dense nutrient poor products eg the ubiquity of fizzy drink vending machines. To that end both Universities in the United States and health services worldwide (see NHS England) are taking the initiative to phase out the sale and promotion of sugary drinks at their sites. At the University of Sydney a group of students, researchers and academics are taking this step through the Sydney University Healthy Beverage Initiative. Check out this fabulous social marketing campaign with indigenous communities in Australia by Rethink Sugary Drink. Sugar-free Smiles advocate for public health policies and regulatory initiatives to reduce sugar consumption and improve the oral health of all Australians. There’s also the Sugar by half campaign.
Key points:
- We need to think about what we are eating.
- Oral health promotion and oral health literacy are important.
- We need to think about the addition of sugar in foods that are ostensibly good for us (cereal and yoghurt for breakfast for example).
The case for working collaboratively: The example of pharmacists
Dr Meng-Wong Taing (Wong) from the University of Queensland persuasively argued how other professionals can have a major role in promoting both oral health and helping to lower the risk of suffering other serious conditions, such as diabetes or cardiovascular disease. Wong cited recent research findings describing the role of Australian community pharmacists in oral healthcare that show 93 per cent of all community pharmacists surveyed believed delivering oral health advice was within their roles as pharmacists. People in lower socio-economic areas often can’t afford to see a dentist and so pharmacies are the first port of call for people experiencing oral health issues. The 2013 ‘National Dental Telephone Interview Survey’, which found the overall proportion of people aged five and over who avoided or delayed visiting a dentist due to cost was 31.7 per cent, ranging from 10.7 per cent for children aged five-14 to 44.9 per cent for people aged 25-44.
Wong’s presentation and those of other speakers over the two days showed the importance of Interprofessional Collaboration (IPC)
IPC occurs when “multiple health workers from different professional backgrounds provide comprehensive services by working with patients, their families, carers, and communities to deliver the highest quality of care across settings” (WHO 2010, p. 13).
Key points:
- How do we get oral health in health professional curricula? Particularly given the emphasis on the technocratic and acute at the expense of health promotion and public health.
- How can we focus on oral health from a broader social determinants perspective?
- Let’s improve access to services and oral health outcomes.
- Let’s develop inter-professional approaches to undergraduate education.
- Let’s develop collaborative approaches and avoiding the ‘siloing’ of oral health.
- Let’s encouraging partnerships between oral health professionals and other health professionals, community groups and advocacy groups.
- Rather than developing better systems, let’s have better relationships that are consumer centred (see above and AUT’s Interprofessional Education and Collaborative Practice (IPECP) website.
Perhaps the best news of the two days for me is that milk, cheese and yoghurt and presumably paneer, contain calcium, casein and phosphorus that create a protective protein film over the enamel surface of the tooth thereby reducing both the risk of tooth decay and the repair of teeth after acid attacks. This information validates my enjoyment of sparkling wine (low sugar but acidic) and cheese. Cheers.